“If you see something, say something.” We hear this phrase all the time in terms of keeping our community safe from potential dangers. As parents, we need to take this same advice to keep our children safe from the risk of suicide and self-harm. If you have any concern that your child may be hurting themselves or thinking about suicide, you can send an email directly to Daybreak and will receive a reply promptly.
Have Questions
Suicide Awareness
Some Facts About Suicide
Suicide is the 2nd leading cause of death for people 10-18 years old. The only more prevalent cause of death were unintentional injury (which includes car accidents, falls, etc). This means that more kids and teenagers died from suicide than from cancer, heart disease, birth defects, stroke, pneumonia, influenza and chronic lung disease combined. The suicide rate for adolescents and teens has increase steadily since 2010.
Females are more likely to attempt suicide and males are more likely to complete suicide.
A 2017 survey showed that nearly 8% of high school students have attempted suicide within the last 12 months. 10% of females had attempted suicide and 5% of males had attempted suicide.
For all age groups, nearly 575,000 people were treated at a hospital for injuries they self inflicted (either suicide attempts that they survived or non-suicidal self injury).
According to the CDC, in 2017 47, 173 Americans died from confirmed suicides. Of these, 23, 854 were from self-inflicted gunshots, 13, 075 died from suffocation, 6,554 from poisoning/overdoses and 3, 690 died from other self-inflicted means. On average, 129 Americans complete suicide each day.
If suicide were any other cause of death other than being self-inflicted there would be no stigma. There would be nothing standing between children and their families and getting the help they need to recover. And, yes, people do recover from suicidal thinking. With proper mental health treatment, children can and do recover from urges to harm themselves and they move past the desire to die.
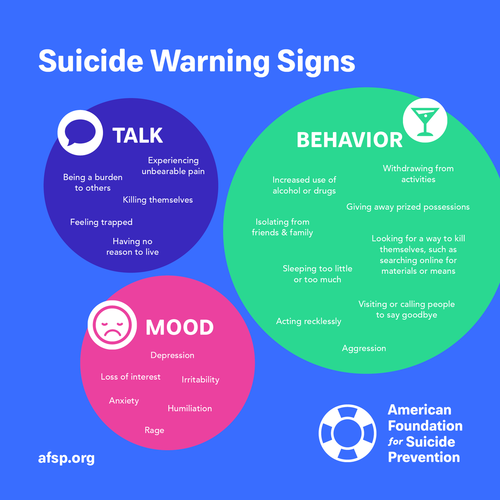
Please read below for more information about red-flags and warning signs that your child may be thinking about hurting themselves or suicide. You are always welcome to call Daybreak at 901-753-4300 for either an evaluation or guidance on how to access help for your child.
Do You Suspect Your Child is Thinking About Waiting to Die?
Has your child said to you that they want to die? Don’t want to be here anymore? Wish they were dead? Wish they had never been born? Don’t want to be a burden/bother anymore? Have they said any of these things to a friend or someone at school? Do they talk about how people would be better of without them? If someone (say the parent of your child’s friend) tells you your child has mentioned wanting to die, treat is as seriously as if you had heard it yourself.
Be aware that kids will also text, snapchat, tweet or otherwise use social media or electronics to share that they are thinking about suicide.
Every time a child says something that indicates they may be thinking about suicide is a time that must be taken seriously. Even a child who is reporting suicidal thinking for “attention-seeking” is at risk to do something to hurt themselves. Also, if your child is making suicidal statements to get attention, there is likely an emotional health need that needs to be explored.
Parents have several options if you suspect your child is contemplating suicide. You can call your child’s outpatient therapist if they have one. You can transport your child to your closest emergency room for a crisis evaluation. You can transport your child to a psychiatric hospital for an evaluation for treatment. You also have the option to call Daybreak, we are happy to provide a no-cost assessment to help you determine if your child can be safely treated on a lower level of care (such as Daybreak, outpatient therapy, or another outpatient program) or if you need to take your child to a hospital to be evaluated for inpatient treatment.
Actions Can Speak Louder Than Words
Sometimes kids are showing us they are thinking about wanting to die, and they haven’t said a word.
Have you noticed that your child is using more alcohol and/or drugs than they used to? Have they started using heavily and recently? Have they stopped doing things that they used to enjoy (quit a sport or club, stopped going to youth group)? Do they spend more time isolated up in their room than they used to? Are they sleeping more (or less) than they did before?
Has your child has a recent loss (death of a loved one, break up of a relationship)? Are they more irritable than normal, are they becoming aggressive toward others? Have they withdrawn from spending time with friends or family? Have you noticed a dramatic change in their personality? Are they less concerned about their hygiene (bathing, brushing teeth, etc)? Are they eating less (or more) than they used to?
Have parents recently separated or divorced? Has something happened to cause them great shame or embarrassment? Are they complaining of physical symptoms of stress (stomach age, headaches, low energy)? Are they in serious trouble for the very first time?
There are also some very “red-flag” behaviors, if any of these occur reach out IMMEDIATELY to a mental health provider:
- giving away special belongings
- contacting people to say good-bye (can be texts, Snapchat, Twitter, etc)
- risky/reckless driving, taking physical chances
- researching ways to kill themselves (look at their on-line search histories)
- preoccupation with death (artwork, essays, poems, etc)
- has your child attempted suicide before (1 out of 2 suicide deaths were NOT the person’s first attempt)
- the risk for completed suicide is 100 times greater within one year of a prior suicide attempt to any intentional self-harm (or an increase in self-harm if is already occurring)
You would never, ever make yourself responsible for determining if your child’s stomachache is severe appendicitis or just a gas bubble that would go away on its own. Please do not put yourself in the position of making such a diagnosis on if your child is at risk for commit suicide. There are trained professionals ready and waiting to help you, and your child, navigate this difficult position.
If you notice these behaviors, especially the “red-flag” behaviors, contact your child’s outpatient therapist immediately. You can also take your child to the closest emergency room for a crisis evaluation or to a psychiatric hospital for an evaluation. You can also call Daybreak for a no cost evaluation to help determine if your child can be safety treated on a lower level of care (such as outpatient therapy or at Daybreak) or if we believe your child needs to be evaluated for inpatient treatment.
Is Your Child Harming Themselves on Purpose
People who injure themselves deliberately, but who are not trying to die, are doing non-suicidal self-injury (NSSI). These children are trying to cope with intense feelings of depression, anxiety, stress, trauma, anger, pain and overwhelm. But, they are often not trying to commit suicide. However, children who do self-harm are more likely to attempt, and complete, suicide than kids who do not self-injure. Therefore, it is very important that we mention self-harm when we talk about being aware of suicide risks for teens.
When we think of self-harming we most often think of girls who cut themselves. It is very important to realize that boys self-harm too!! Self-harming can happen by cutting, burning, pinching and hitting oneself. It can also be banging the head against the wall and punching things (yes, what looks like anger can in fact be self-harming). It can also be picking at wounds so they never heal, peeling fingernails/cuticles and having accidents that aren’t accidents at all (falls, shutting hands in doors, etc). Running away from home and restricting food intake are also self-harming behaviors. So is risky driving.
Kids who self harm do so for many reasons, only a mental health professional can determine what the reasons are and help your child process through them. It is important to remember that your child is using self-harming as a coping skills and continues to do it because on some level, it is working for them. They are trapped in the self-harm cycle in the graphic to the left.
By the time you know that an incident of self-harming has occurred, there are likely several incidents you don’t know about. If you come to know, or suspect, your child is hurting themselves on purpose, you can call your outpatient therapist. Or, you can call Daybreak and we will help connect you with a qualified therapist in the community. Sometimes, self-harming is so intense and dangerous that your child might require more intensive treatment. Daybreak can help you figure that out as well.